CSP Statement on the Physician-Assisted Death legislation in Canada
The Centre for Suicide Prevention (CSP)
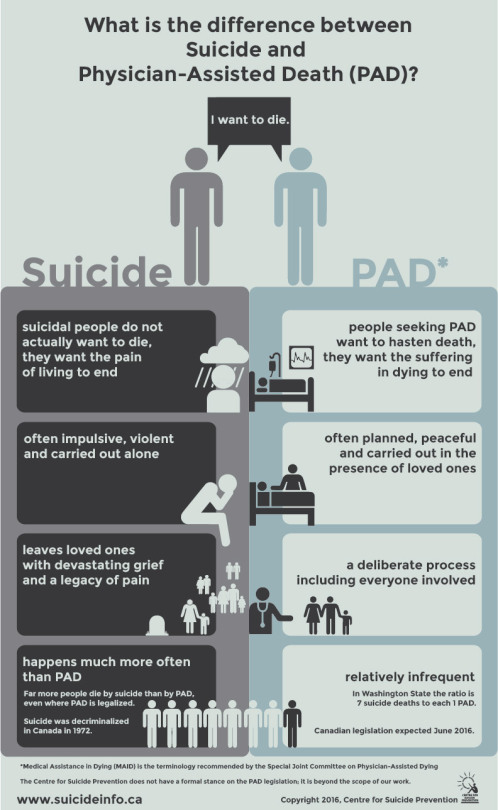
urges the Government of Canada to make a clear distinction between physician-assisted
death (PAD) and suicide. Though often used interchangeably, these are two
different issues that affect two distinct groups of people. It would be
disastrous if, by attempting to help Canadians seeking medical
assistance in dying, Canadians
experiencing suicidality are further stigmatized. Distinguishing between these two
populations with clarity of language is paramount.
Nearly all people who consider,
attempt and/or die by suicide do not want to die: they want the pain of living
to end. When they are at a point of suicidal crisis, they cannot see
alternatives to their situation beyond death. Given help, they will choose
help. Suicidality is temporary: people can be at immediate risk of suicide,
then not, then experience a suicide crisis again. Others may only have one
suicidal experience in their lifetime. With appropriate mental health care,
people who have experienced suicidality can go on to live mentally healthy
lives: recovery is possible. Others learn how to live with their suicidality,
often with the support of others around them.
Far more people die by suicide than
by medical assistance in dying even
where PAD is legalized. In Washington, for example, the ratio of
physician-assisted deaths to suicide deaths is roughly 1:7.
As part of the implementation of physician-assisted
death legislation, CSP urges the Government of Canada to educate Canadians
about the distinction between these two groups to help protect those people
experiencing suicidality. People experiencing suicidality often do not seek
help even though they want it. If death becomes a normalized option, Canadians
may become less knowledgeable, sensitive and likely to help those in need.
Infographic References
American Association of Suicidology. USA. Suicide: 2013 Official Final Data. Retrieved from http://www.suicidology.org/portals/14/docs/resources/factsheets/2013datapgsv2alt.pdf
Brody, H. (1995). Physician-assisted suicide: Family issues.
Michigan Family Review, 1(1), 19-28.
de Groot, M., et al. (2007). Cognitive behaviour therapy to prevent
complicated grief among relatives and spouses bereaved by suicide: Cluster
randomized trial. BMJ. DOI:
10.1136/bmj.39161.457431.55
Giner, et al. (2013). Violent and serious suicide attempters: One
step closer to suicide? Journal of
Clinical Psychiatry, 75(3).
Gvion, et al. (2015). On the
role of impulsivity and decision-making in suicidal behavior. World Journal of Psychiatry, 5(3),
255-259.
Jimenez-Trevino, L. (2015). Factors associated with hospitalization
after suicide spectrum behaviors: Results from multicenter study in Spain. Archives of Suicide Research, 19(1),
17-34.
Loy, M. and Boelk, A. (2014). Losing
a parent to suicide: Using lived experiences to inform bereavement counseling.
New York: Routledge.
Shneidman. E. (1993). Suicide as psychache: A clinical approach to
self-destructive behavior. Northvale, NJ.: Jason Aronson, Inc.
Washington State Department of Health. (2014). 2014 Death with
Dignity Act Report: Executive Summary. Retrieved from http://www.doh.wa.gov/portals/1/Documents/Pubs/422-109-DeathWithDignityAct2014.pdf